The Health Enhancement Program (HEP) is a voluntary program that helps you save money on healthcare by following simple guidelines for preventive care and managing chronic conditions. Finding health issues early can lead to better health and savings to help keep the state’s comprehensive coverage and low copays.
“HEP saved my life after a required mammogram revealed evidence of a deep tumor. My breast cancer was treated, and I am now cancer-free”
–HEP participant
About HEP
It promotes regular check-ups and screenings to catch health issues early and ensure you receive timely care, while reducing your out-of-pocket costs.
HEP keeps health plan costs manageable for everyone.
By completing your age-related screenings and any required education for chronic conditions each year, you save on healthcare costs. If everyone covered under your plan does not meet these requirements, you will have an in-network deductible of up to $1,400 and your monthly premiums will increase by $100 per month.
If you’re a State Employee or Retiree enrolling in benefits for the first time, you’ll be automatically enrolled in HEP unless you opt-out. If you wish to opt out of HEP, you must do so during the first 31 days of hire or the annual open enrollment. State Employees must complete Form CO-1316 and send it to your Agency Benefits Specialist.
Partnership employees may not opt out of HEP and incur higher premiums if non-compliant.
HEP compliance is measured once you are in the program for a full calendar year. For example, if the effective date of your insurance is Jan. 1, 2025, you must be compliant by Dec. 31, 2025. If the effective date of your insurance is July 1, 2025, you must be compliant by Dec. 31, 2026.
HEp Requirements
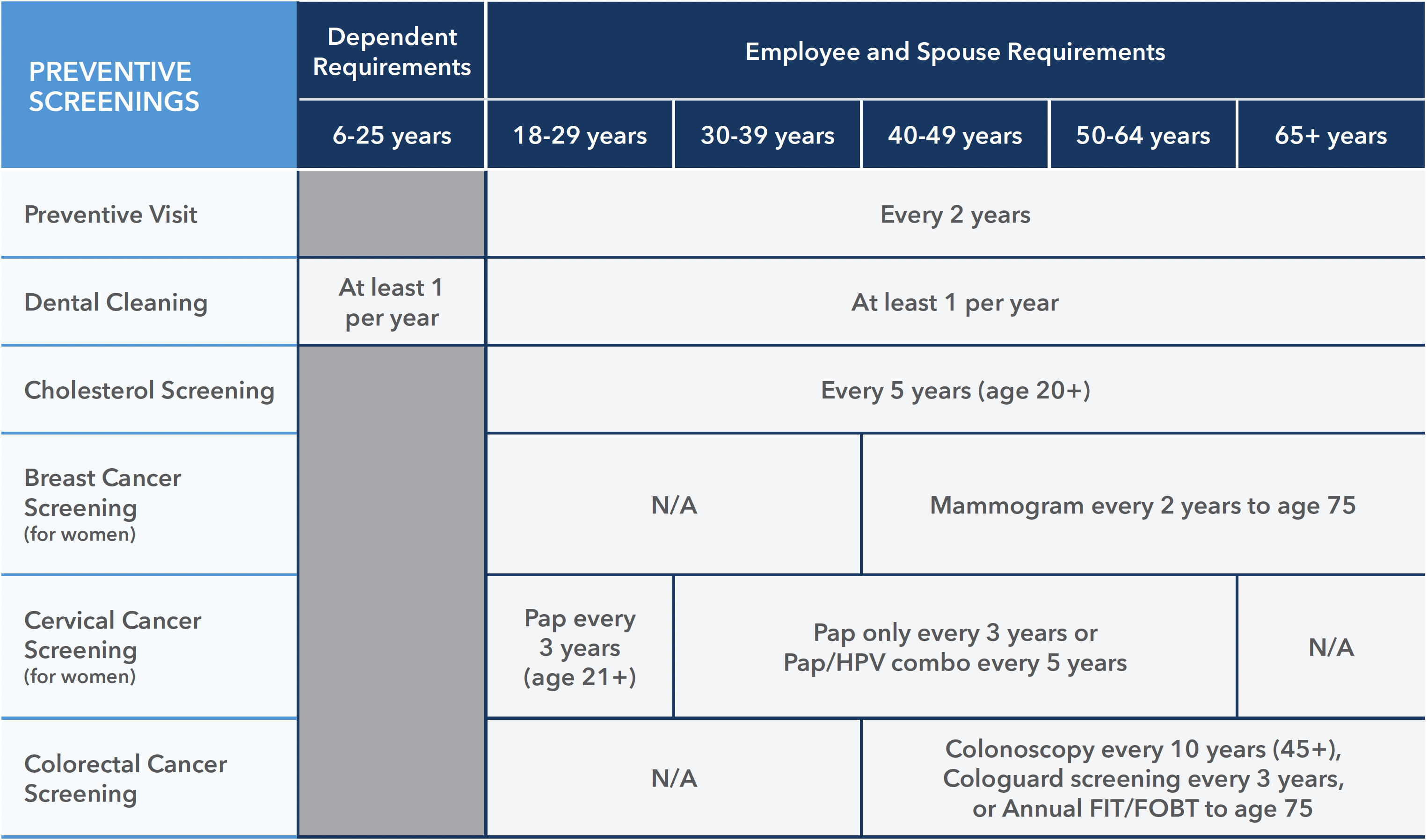
HEP participants must complete certain preventive care requirements that promote early detection of health issues.
The HEP portal is now live. Check your status. (To view your current compliance status, select the current year.)
Specific requirements vary based on age, gender, and health status, aligning with the latest U.S. Preventive Services Task Force recommendations. Participants are provided with detailed guidelines on what is needed each year.
Get paid to stay on track: If you have a colonoscopy requirement, choosing a GI specialist listed as a Provider of Distinction in the search tool will earn you a $100 incentive while completing this HEP requirement.
Chronic Conditions*:
You and/or your family members will be required to participate in a disease education and counseling program if you have:
- Diabetes (type 1 or 2)
- Asthma or COPD
- Heart disease/heart failure
- Hyperlipidemia (high cholesterol)
- Hypertension (high blood pressure)
*Note: This is an annual requirement due by December 31st, along with your preventive requirements. You will receive free office visits and reduced pharmacy copays for treatments related to your condition. Your household must meet all preventive and chronic requirements to be compliant.
To meet the chronic education requirement, complete one of the following options:
- Take a short survey
- Read a fact sheet
- Register & attend a Wellbeing Seminar specific to your condition
HEP resources
- HEP Seminar Schedule
- Frequently Asked Questions (ENGLISH) (Spanish)
- 2026 HEP Handout
Reminder: Complete your HEP requirements by December 31! Need help or have questions? Contact a Care Coordinator at 833-740-3258 for assistance.
“My husband’s mandatory colonoscopy led to an early colon cancer diagnosis, allowing for timely treatment. I truly believe HEP saved his life.”
–HEP Participant
